T
R
A
C
K
M
E
 The non-stop gain
The non-stop gain Investigators at The Feinstein Institute for Medical Research have discovered a new genetic risk factor for schizophreniaand bipolar disorder called NDST3. The findings are published online in Nature Communications.
Investigators at The Feinstein Institute for Medical Research have discovered a new genetic risk factor for schizophreniaand bipolar disorder called NDST3. The findings are published online in Nature Communications.
The study, by a team lead by Todd Lencz, PhD, associate investigator at the Zucker Hillside Hospital Department of Psychiatry Research and Feinstein Institute, studied more than 25,000 individuals. In collaboration with Ariel Darvasi, PhD, of the Hebrew University of Jerusalem, Dr. Lencz has been working with a set of DNA samples from patients with schizophrenia and healthy volunteers drawn from the Ashkenazi Jewish population. The Ashkenazi Jewish population represents a unique population for study because of its short (less than 1,000-year) history and limited population. This history results in a more uniform genetic background in which to identify disease-related variants.
“This study again demonstrates the value of our Ashkenazi cohort,” said Dr. Lencz. “It is notable that the genetic variant was replicated in samples of various ethnicities from all around the world, but the effects were strongest in the Ashkenazi cohort, presumably due to their unique genetic history.”
Dr. Lencz’s team reported that the genetic variant, which changes a single “letter” of the DNA code, alters the expression of the gene NDST3. This gene is critical to neurodevelopmental processes such as axon formation and synaptic function. These findings shed new light on the genetic architecture and potential therapeutic targets for the treatment of psychiatric disease.
Schizophrenia and bipolar disorder are severe psychiatric disorders that affect 1-4 percent of the global population. Studies have shown that the two disorders are likely to have a large overlap in genetic risk factors, but only a small portion of this genetic risk has been identified.
This work was supported by a grant from the National Institute of Mental Health (NIMH), funded as part of the American Recovery and Reinvestment Act of 2009 (also known as the economic stimulus plan). More recently, the work by Drs. Lencz and Darvasi with the Ashkenazi schizophrenia cohort has received an additional $3 million from the NIMH, as well as grants from the Brain & Behavior Foundation and the Binational Science Foundation.
Dr. Lencz is also the co-leader of The Ashkenazi Genomics Consortium, a collaborative effort involving more than a dozen investigators from leading institutions (including Columbia University, Mt. Sinai School of Medicine, Albert Einstein College of Medicine and MIT), using similar strategies to understand the genetic basis of diseases including cancer, diabetes, and Parkinson’s.
 The use of antidepressants in the treatment of bipolar disorder remains controversial. Some studies and treatment guidelines suggest that antidepressant treatment for bipolar disorder may have the potential to increase the manic switch, while others recommend short-term antidepressant treatment and early discontinuation. A recent study by Dr. Yingli Zhang and co-workers from Mental Health Institute of Central South University in China involved new large-sample double-blind randomized controlled trials, excluded open-label design studies, and supplemented studies involving homogeneous patients. Suicidality firstly served as an important outcome, strict inclusion criteria included limitation to double-blind randomized controlled studies and interventional treatment without use of antipsychotics to make the study results more objective and convincing. The results from this study do not support that antidepressants are more effective in the treatment of bipolar disorder. Antidepressants are not superior to placebo and other medication in short-term, and long-term use of antidepressants cannot achieve higher response and remission rates of bipolar disorder. These findings, published in the Neural Regeneration Research (Vol. 8, No. 31, 2013), guide future clinical studies and provide evidence for preparing treatment strategy for bipolar disorder.
The use of antidepressants in the treatment of bipolar disorder remains controversial. Some studies and treatment guidelines suggest that antidepressant treatment for bipolar disorder may have the potential to increase the manic switch, while others recommend short-term antidepressant treatment and early discontinuation. A recent study by Dr. Yingli Zhang and co-workers from Mental Health Institute of Central South University in China involved new large-sample double-blind randomized controlled trials, excluded open-label design studies, and supplemented studies involving homogeneous patients. Suicidality firstly served as an important outcome, strict inclusion criteria included limitation to double-blind randomized controlled studies and interventional treatment without use of antipsychotics to make the study results more objective and convincing. The results from this study do not support that antidepressants are more effective in the treatment of bipolar disorder. Antidepressants are not superior to placebo and other medication in short-term, and long-term use of antidepressants cannot achieve higher response and remission rates of bipolar disorder. These findings, published in the Neural Regeneration Research (Vol. 8, No. 31, 2013), guide future clinical studies and provide evidence for preparing treatment strategy for bipolar disorder.
THE SAINT THEY CALLED ALLNIGHTS
I was somewhat confused at this one and like the last just kept ignoring it.
But them I did hear a but about how the Police will need help, yup tying their shoelaces, from mental health staff.
Well as it has now been five years since they were cut loose from all support whatsoever and now gradually being wound up while staining the streets stealing from people and shops, attacking people and killing people then YEAH the Police need help.
Of course like everything else it will all be put back to how it should have been left in the first place. But first it has to be someone rich or famous that suffers at the hands of there incompetent stupidity before it does?!
Or someone that matters in other words.
Sad but true and someone stated to be that mentally challenged and unstable people can work?! I said oh…
View original post 263 more words
 “Here is the Hope that you’re looking for. Here is the Truth you need” promises author Liz Curtis Higgs.
“Here is the Hope that you’re looking for. Here is the Truth you need” promises author Liz Curtis Higgs.
Quite a promise for a book I haven’t started yet. The praise for Sheila Walsh’s newest book goes on for three pages at the front, with names as big as Amy Grant and Joni Eareckson Tada applauding it. Even Kay Warren, who lost her son to suicide last year, says “Sheila understands.”
I’ve been given the privilege to be a part of the launch team for Shelia’s latest book: The Storm Inside: Trade the chaos of how you feel for the truth of who you are. Part of this privilege is the opportunity to read the book earlier than everyone else and let other people know what I think of it.
I’m a huge fan of Sheila Walsh, but even I wasn’t sure that she could achieve what the…
View original post 302 more words

For several years I wrote poetry every day, feverishly. I felt like I would explode if I didn’t write the words in my brain. It was as if I was taken over by a force outside of myself, and what I ended up writing was as much as a surprise to me as it would have been to a stranger reading it. Exciting and energizing are the best words to describe the experience of writing poetry for me.
I loss the ability to access this side of my creativity about a year ago. It coincided with the time I started a new antipsychotic medication for my anxiety. I don’t know for sure if my creativity block has to do with the medication, but I strongly suspect it does.
I also experienced large amounts of emotional healing during that year, which may have contributed to the end of my drive to…
View original post 134 more words

Outpatient Mental Health Clinic Pt. 1
A sort of chaos pervades this place. It underscores the fact that lumping people with varying mental illnesses together at what is likely to be their lowest point is like herding kittens.
Only these kittens are blind from birth, hit by a car and have managed to survive. They start new patients as early as possible which means new people are coming in every day, shell-shocked, withdrawn and hopeless. And every day veterans leave, mostly with a renewed confidence and readiness to grapple with their mental illness and the world.
It’s my first day there and 30 people have wedged themselves in a classroom with a big square table in the middle. I find an empty spot because having just met with my therapist Beth, I am tardy. Thus begins the confusion. I have no idea what the hell is going on.
I have been…
View original post 309 more words
Super Glue & Duct Tape ...holding it all together!
It’s 4:13 in the afternoon. I’m still sitting on the couch. I finally decided to force feed myself after 3 or 4 days and still not hungry at all. So, I shoved some Ramen Noodles into my belly whether I liked it or not. My hubby is still gone and I really need him to be here. More than that, when he is here I need him to help me pull out of this – or take me to the damn hospital…it’s been too long. Another 4 days without a shower, just changed my clothes because I started to smell myself. Thank God my boy is over at a friends for the weekend. I don’t even half to get up and feed him. I can just sit, sit, sit, sit, sit. I feel like I am rotting.
It was inevitable I guess. After so many trial and errors with medication, it was no longer possible to avoid the elephant in the room. I was not responding to medication and this was the next logical treatment option. But just the thought of it makes me want to barf.
The topic had come up a few times with my doc but he always hesitated citing how important he felt my “clear mindedness” meant to me. He was worried that losing my short term memory, one of the side effects of ECT (electroconvulsive therapy), would be distressing and cause me even more anxiety that I was already trying to cope with. But with each medication we tried, my hopes were quickly dashed due to my lack of response. Even though the thought of going through ECT scares the hell out me, the thought of feeling this way for the rest…
View original post 263 more words
Problems, people hate having them yet we love knowing the causes of them. Why write about them? When mental health is diagnosed, it brings a whole system of attention to the diagnosed family member. The entire family is caught up around accepting, understanding and helping. The entire focus of the household is shifted away from the family as a unit and to healing an individual – whom is treated or cared for by CPNs, doctors and psychologists. They are a presence in the lives of the family, yet mental health and its effects on the children of patients remains undocumented by comparison.
Mom left me when I was six years old. She moved to Wales with her drug-dealing boyfriend and gave birth to my half-sister. I saw both two-three times a year. Her partner ignored me. When ten, my sister died of cot-death. There was suspected abuse, and cannabis was…
View original post 1,327 more words
 After visiting family in Wisconsin, a place where cold people have warm hearts, it is good to return to our home in Southern Illinois. I have been thinking about what my next blog would be. The answer became clear while I was surfing over the internet and discovered a blog that grabbed my attention. Because of time restraints, I do not follow a large number of blogs. But this one caused me to quickly click the “follow” button. The blog, “Weathering the Storm: Overcoming Bipolar Disorder,” is truly remarkable, and is written by Kait Leigh, a young lady who has bipolar disorder. Kait’s life is one of overcoming the struggles brought on by mental illness, particularly bipolar disorder. Even if you or a family member do not suffer from bipolar disorder, you should check out her blog, http://weatheringthestormbp.com/contact/ Where her story is filled with the blackness of night, she has…
After visiting family in Wisconsin, a place where cold people have warm hearts, it is good to return to our home in Southern Illinois. I have been thinking about what my next blog would be. The answer became clear while I was surfing over the internet and discovered a blog that grabbed my attention. Because of time restraints, I do not follow a large number of blogs. But this one caused me to quickly click the “follow” button. The blog, “Weathering the Storm: Overcoming Bipolar Disorder,” is truly remarkable, and is written by Kait Leigh, a young lady who has bipolar disorder. Kait’s life is one of overcoming the struggles brought on by mental illness, particularly bipolar disorder. Even if you or a family member do not suffer from bipolar disorder, you should check out her blog, http://weatheringthestormbp.com/contact/ Where her story is filled with the blackness of night, she has…
View original post 422 more words
After my mother texted me yesterday to tell me I had to read Nicholas Kristof’s New York Times Sunday op-ed — “First Up, Mental Illness. Next Topic Is Up to You“– I didn’t drop everything to read it right away because she recommends a lot of articles to me. But then — Amen! That’s what I wanted to shout out my window when I read it this morning.
Kristof writes:
My own suggestion for a systematically neglected issue: mental health. One-quarter of American adults suffer from a diagnosable mental disorder, including depression, anorexia, post-traumatic stress disorder and more, according to the National Institutes of Health. Such disorders are the leading cause of disability in the United States and Canada, the N.I.H. says.
A parent with depression. A lover who is bipolar. A child with an eating disorder. A brother who returned from war with P.T.S.D. A sister…
View original post 363 more words
So the big day is tomorrow…
Tomorrow early morning to be more precise. So by the time you’re probably reading this it’ll be a done deal.
This means I’m writing this prior to being brain buzzed for the first time, so we’ll call this BEFORE.
Therefore anything prior to January 6, say 8-9 in the morning, if also BEFORE. And if you know me up to this point, same deal.
If you notice any big difference in me in the next few weeks, let me know. I apparently have to get this done a few times before they know if it’s working. Tomorrow is the first of 3 for this week. I have marked them with little Shazam lightning bolts on my “Batman 66” calendar. I know it’s a little sick, but that’s kind of the point, right?
No. The point is trying to get back to being a more…
View original post 304 more words
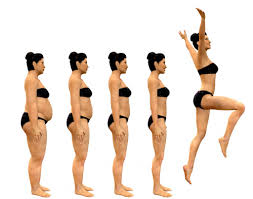
 People with serious mental illnesses such as schizophrenia, bipolar disorder and major depression can lose weight and keep it off through a modified lifestyle intervention program, a National Institute of Mental Health (NIMH)-funded study reported online today in The New England Journal of Medicine.
People with serious mental illnesses such as schizophrenia, bipolar disorder and major depression can lose weight and keep it off through a modified lifestyle intervention program, a National Institute of Mental Health (NIMH)-funded study reported online today in The New England Journal of Medicine.
Over 80 percent of people with serious mental illnesses are overweight or obese, which contributes to them dying at three times the rate of the overall population. They succumb mostly to the same things the rest of the population experiences—cardiovascular disease, diabetes and cancer. Although antipsychotic medicationsincrease appetite and cause weight gain in these patients, it is not the only culprit. Like the general population, sedentary lifestyle and poor diet also play a part. Lifestyle modifications such as diet and exercise should work for these patients, yet they are often left out of weight loss studies.
“People with serious mental illnesses are commonly excluded from studies to help them help themselves about their weight, said Gail L. Daumit, M.D., of Johns Hopkins University, Baltimore, and the study’s lead author. “We’re showing that serious mentally ill patients can make successful, sustained changes with proper interventions.”
This study could usher in new forms of weight loss treatment for people with serious mental illness.
“Until now, obesity among those with serious mental illnesses has not received adequate attention,” said NIMH Director Thomas R. Insel, M.D. “People with serious mental illnesses need more attention to their physical health. This study provides convincing evidence these individuals can make substantial lifestyle changes and therefore should suffer fewer medical complications as they age.”
Other factors that preclude people with serious mental illnesses from losing weight include memory impairments or residual psychiatric symptoms that impede learning and adopting new behaviors such as counting calories. Socioeconomics are also a factor as many can’t afford or can’t get to physical activity programs like fitness gyms. Some patients additionally suffer from social phobia or have poor social interactions, and are simply afraid to work out in a public area.
Daumit’s group attempted to solve these issues by bringing the gyms and nutritionists to places most of these patients frequent—psychiatric rehabilitation outpatient programs. Under the trial nameACHIEVE, the researchers randomized 291 participants in 10 rehab centers around Maryland to receive the usual care, consisting of nutrition and physical activity information, or six months of intensive intervention consisting of exercise classes three times a week along with individual or group weight loss classes once a week. Both groups were followed for an additional year, during which the weight loss classes of the intervention arm tapered down but the exercise classes remained constant. The intervention arm included goals such as reducing caloric intake by avoiding sugar-sweetened beverages and junk food; eating five servings of fruits and vegetables daily; choosing smaller portions and healthy snacks; and moderate intensity aerobic exercise.
Participants in the specially tailored weight loss program lost seven pounds more than the controls—and continued to lose weight and did not regain, despite the reduced frequency of classes and counseling sessions. In contrast, the general population tends to experience peak weight loss in the first six months and then rebound and gain part or all of their weight back.
On average, each participant was on three psychotropic medications, with half on lithium or mood stabilizers, all known to cause weight gain. But no matter what they were on, they lost the weight.
“We’re showing behavioral interventions work regardless of what they’re taking,” Daumit said. Her group is now looking for ways to spread the program.
Effects of a behavioral weight loss intervention in persons with serious mental illness. Daumit GL, Dickerson FB, Wang N-Y, Dalcin A, Jerome GJ, Anderson CAM, Young DR, Frick KD, Yu A, Gennusa III JV, Oefinger M, Crum RM, Charleston J, Casagrande SS, Guallar E, Goldberg RW, Campbell LM, Appel LJ. NEJM, March 21, 2013.
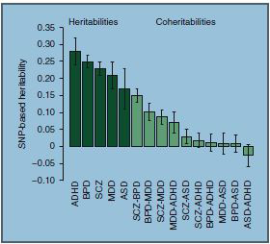 The largest genome-wide study of its kind has determined how much five major mental illnesses are traceable to the same common inherited genetic variations. Researchers funded in part by the National Institutes of Health found that the overlap was highest between schizophrenia and bipolar disorder; moderate for bipolar disorder and depression and for ADHD and depression; and low between schizophrenia and autism. Overall, common genetic variation accounted for 17-28 percent of risk for the illnesses.
The largest genome-wide study of its kind has determined how much five major mental illnesses are traceable to the same common inherited genetic variations. Researchers funded in part by the National Institutes of Health found that the overlap was highest between schizophrenia and bipolar disorder; moderate for bipolar disorder and depression and for ADHD and depression; and low between schizophrenia and autism. Overall, common genetic variation accounted for 17-28 percent of risk for the illnesses.
“Since our study only looked at common gene variants, the total genetic overlap between the disorders is likely higher,” explainedNaomi Wray, Ph.D., University of Queensland, Brisbane, Australia, who co-led the multi-site study by the Cross Disorders Group of the Psychiatric Genomics Consortium (PGC), which is supported by the NIH’s National Institute of Mental Health (NIMH). “Shared variants with smaller effects, rare variants, mutations, duplications, deletions, and gene-environment interactions also contribute to these illnesses.”
Dr. Wray, Kenneth Kendler, M.D., of Virginia Commonwealth University, Richmond, Jordan Smoller, M.D., of Massachusetts General Hospital, Boston, and other members of the PGC group report on their findings August 11, 2013, in the journal Nature Genetics.
“Such evidence quantifying shared genetic risk factors among traditional psychiatric diagnoses will help us move toward classification that will be more faithful to nature,” said Bruce Cuthbert, Ph.D., director of the NIMH Division of Adult Translational Research and Treatment Development and coordinator of the Institute’sResearch Domain Criteria (RDoC) project, which is developing a mental disorders classification system for research based more on underlying causes.
Earlier this year, PGC researchers – more than 300 scientists at 80 research centers in 20 countries – reported the first evidence of overlap between all five disorders. People with the disorders were more likely to have suspect variation at the same four chromosomal sites. But the extent of the overlap remained unclear. In the new study, they used the same genome-wide information and the largest data sets currently available to estimate the risk for the illnesses attributable to any of hundreds of thousands of sites of common variability in the genetic code across chromosomes. They looked for similarities in such genetic variation among several thousand people with each illness and compared them to controls – calculating the extent to which pairs of disorders are linked to the same genetic variants.
The overlap in heritability attributable to common genetic variation was about 15 percent between schizophrenia and bipolar disorder, about 10 percent between bipolar disorder and depression, about 9 percent between schizophrenia and depression, and about 3 percent between schizophrenia and autism.
The newfound molecular genetic evidence linking schizophrenia and depression, if replicated, could have important implications for diagnostics and research, say the researchers. They expected to see more overlap between ADHD and autism, but the modest schizophrenia-autism connection is consistent with other emerging evidence.
The study results also attach numbers to molecular evidence documenting the importance of heritability traceable to common genetic variation in causing these five major mental illnesses. Yet this still leaves much of the likely inherited genetic contribution to the disorders unexplained – not to mention non-inherited genetic factors. For example, common genetic variation accounted for 23 percent of schizophrenia, but evidence from twin and family studies estimate its total heritability at 81 percent. Similarly, the gaps are 25 percent vs. 75 percent for bipolar disorder, 28 percent vs. 75 percent for ADHD, 14 percent vs. 80 percent for autism, and 21 percent vs. 37 percent for depression.
Among other types of genetic inheritance known to affect risk and not detected in this study are contributions from rare variants not associated with common sites of genetic variation. However, the researchers say that their results show clearly that more illness-linked common variants with small effects will be discovered with the greater statistical power that comes with larger sample sizes.
“It is encouraging that the estimates of genetic contributions to mental disorders trace those from more traditional family and twin studies. The study points to a future of active gene discovery for mental disorders” said Thomas Lehner, Ph.D., chief of the NIMH Genomics Research Branch, which funds the project.
Common inherited genetic variation (single nucleotide polymorphisms, or SNPs) accounted for up to about 28 percent of the risk for some disorders, such as ADHD (dark green). Among pairs of disorders (light green), schizophrenia and bipolar disorder (SCZ-BPD) shared about 16 percent of the same common genetic variation (coheritabilities).
Source: Cross-Disorder Group of the Psychiatric Genomics Consortium
Cross-Disorder Group of the Psychiatric Genomics Consortium. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nature Genetics, August 11, 2013
 Oct. 2, 2013 — A study published in the October 2013 issue of the Journal of the American Academy of Child and Adolescent Psychiatry found that approximately one in three teens with bipolar disorder developed substance abuse, for the first time, during 4 years of follow-up. The study also identified several risk factors that predicted who among these teens was most likely to develop substance abuse.
Oct. 2, 2013 — A study published in the October 2013 issue of the Journal of the American Academy of Child and Adolescent Psychiatry found that approximately one in three teens with bipolar disorder developed substance abuse, for the first time, during 4 years of follow-up. The study also identified several risk factors that predicted who among these teens was most likely to develop substance abuse.
Using data from the Course and Outcome of Bipolar Youth (COBY) study, a group of researchers led by Dr. Benjamin Goldstein, of the University of Toronto and the University of Pittsburgh, examined 167 youth, ages 12-17 years, to document the frequency and possible predictors of first-onset substance abuse. Participants in the study were interviewed an average of 7 times over the course of 4 years in order to examine their symptoms, functioning, stressors, and treatment.
The study found that 32% of adolescents in COBY developed abuse or dependence of alcohol or drugs, on average 2.7 years from the start of the study. Repeated experimentation with alcohol at the start of the study was the single strongest predictor of later substance abuse, although experimentation with cannabis also predicted later substance abuse. Five other factors present at the start of the study also predicted later substance abuse: oppositional defiant disorder, panic disorder, family history of substance abuse, low family cohesiveness, and absence of antidepressant treatment. Among teens with 3 or more risk factors, 54.7% went on to develop substance abuse, compared to 14.1% of teens with 0-2 risk factors.
The COBY study, funded by the National Institute of Mental Health, is the largest longitudinal study of children and adolescents with bipolar disorder. The 3-site study enrolled participants at Brown University, UCLA, and the University of Pittsburgh. COBY is continuing to follow these adolescents into their twenties and thirties.
Dr. Goldstein highlighted the risk associated with experimental substance use “in the case of adolescents with bipolar disorder, even so-called recreational substance use is playing with fire.” He concluded “we appear to have this window of 2-3 years during which we can attempt to prevent substance abuse in these youth. This study provides some clues regarding the types of preventive strategies that may be useful.”
Journal Reference:
Benjamin I. Goldstein, Michael Strober, David Axelson, Tina R. Goldstein, Mary Kay Gill, Heather Hower, Daniel Dickstein, Jeffrey Hunt, Shirley Yen, Eunice Kim, Wonho Ha, Fangzi Liao, Jieyu Fan, Satish Iyengar, Neal D. Ryan, Martin B. Keller, Boris Birmaher. Predictors of First-Onset Substance Use Disorders During the Prospective Course of Bipolar Spectrum Disorders in Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 2013; 52 (10): 1026 DOI:
Nov. 1, 2013 — New Northwestern Medicine® research offers one of the first in-depth studies of how physiological changes during pregnancy reduce the effects of a commonly used drug to treat bipolar disorder, making women more vulnerable to recurring episodes. The new findings will help psychiatrists and physicians prevent bipolar manic and depressive symptoms during pregnancy, which are risky for the health of the mother and her unborn child.
When a woman with bipolar disorder becomes pregnant, she and her physician often don’t realize her medication needs adjusting to prevent the symptoms from coming back — a higher risk during pregnancy. There also is little information and research to guide dosing for psychiatric medications during pregnancy.
Approximately 4.4 million women in the U.S. have bipolar disorder with women of childbearing age having the highest prevalence.
The new study shows the blood concentration of the commonly used drug lamotrigine decreases in pregnant women. About half of the women in the study had worsening depressive symptoms as their lamotrigine blood levels dropped. The drug levels fall because women have increased metabolism during pregnancy.
“Now physicians change the dose of the drug in response to women’s symptoms worsening,” said lead investigator Crystal Clark, M.D., an assistant professor of psychiatry and behavioral sciences at Northwestern University Feinberg School of Medicine and a psychiatrist at Northwestern Memorial Hospital. “We need to optimize their medication dosing so they stay well.”
The study results will help physicians understand how to increase their patients’ doses during pregnancy and then reduce them postpartum to avoid toxicity, Clark said. Guidelines for prescribing the drug for pregnant women with the disorder also are included.
The study was published Nov. 1 in the American Journal of Psychiatry.
Depressive episodes — as opposed to manic — are most likely to recur in pregnant women with bipolar disorder.
“The safety of the fetus is at risk,” Clark said. “Pregnant women that are depressed are less likely to take care of themselves which often leads to poor nutrition, lack of compliance with prenatal care and isolation from family and friends. It has also been linked to premature births and babies with low birth weights among other poor birth outcomes.”
Reference: Crystal T. Clark. Lamotrigine Dosing for Pregnant Patients With Bipolar Disorder. American Journal of Psychiatry, 2013; 170 (11): 1240 DOI:
<img alt=”Donate Button with Credit Cards” src=”https://www.paypal.com/en_US/i/btn/btn_donateCC_LG.gif” />
The person in this video touched my heart. Share my feelings.
| A Short Bipolar Disorder Summary | |||
| Bipolar disorder, is a serious brain disorder. Also known as manic-depressive illness, it is a mental illness involving episodes of serious mania and depression. The person’s mood usually swings from overly “high” and irritable to sad and hopeless, and then back again, with periods of normal mood in between.
Bipolar disorder typically begins in adolescence or early adulthood and continues throughout life. It is often not recognized as an illness and people who have it may suffer needlessly for years or even decades.
Facts about bipolar disorder:
Signs and Symptoms
It may be helpful to think of the various mood states in manic-depressive illness as a spectrum or continuous range. At one end is severe depression, which shades into moderate depression; then come mild and brief mood disturbances that many people call “the blues”, then normal mood, then hypomania (a mild form of mania), and then mania. Recognition of the various mood states is essential so that the person who has manic-depressive illness can obtain effective treatment and avoid the harmful consequences of the disease, which include destruction of personal relationships, loss of employment, and suicide. Manic-depressive illness is often not recognized by the patient, relatives, friends, or even physicians. An early sign of manic-depressive illness may be hypomania–a state in which the person shows a high level of energy, excessive moodiness or irritability and impulsive or reckless behavior. Hypomania may feel good to the person who experiences it. Thus even when family and friends learn to recognize the mood swings the individual often will deny that anything is wrong. In its early stages bipolar disorder may masquerade as a problem other than mental illness. For example, it may first appear as alcohol or drug abuse, or poor school or work performance. If left untreated, bipolar disorder tends to worsen and the person experiences episodes of full-fledged mania and clinical depression. Descriptions offered by patients themselves offer valuable insights into the various mood states associated with bipolar disorder:
TreatmentAlmost all people with bipolar disorder–even those with the most severe forms–can obtain substantial stabilization of their mood swings. One medication, lithium, is usually very effective in controlling mania and preventing the recurrence of both manic and depressive episodes. More recently, the mood-stabilizing anticonvulsants carbamazepine and valproate have also been found useful especially in more refractory bipolar episodes. Often these medications are combined with lithium for maximum effect. Some scientists have theorized that the anticonvulsant medications work because they have an effect on kindling, a process in which the brain becomes increasingly sensitive to stress and eventually begins to show episodes of abnormal activity even in the absence of a stressor. It is thought that lithium acts to block the early stages of this kindling process and that carbamazepine and valproate act later. Valproate has recently been approved by the Food and Drug Administration for treatment of acute mania. Children and adolescents with bipolar disorder are generally treated with lithium, but carbamazepine and valproate are also used. The high potency benzodiazepines; clonazepam and lorazepam may be helpful adjuncts for insomnia. Thyroid augmentation may also be of value. For depression, several types of antidepressants can be useful when combined with lithium, carbamazepine or valproate. Electroconvulsive therapy (ECT) is often helpful in the treatment of severe depression and/or mixed mania that does not respond to medications. As an adjunct to medications, psychotherapy is often helpful in providing support, education, and guidance to the patient and his or her family. Constructing a life chart of mood symptoms, medications, and life events may help the health care professional to treat the illness optimally. Because manic-depressive illness is recurrent, long-term preventive (prophylactic) treatment is highly recommended and almost always indicated. Some people with untreated bipolar disorder have repeated depressions and only an occasional episode of hypomania (bipolar II). In the other extreme, mania may be the main problem and depression may occur only infrequently. In fact, symptoms of mania and depression may be mixed together in a single bipolar state. This information has been excerpted from material developed by the National Institute for Mental Health. Please Click HERE to see my products page. There are some bipolar products and also many other products. Make a Difference. |
Lee Thompson Young suffered from bipolar disorder, coroner says
LOS ANGELES, Oct. 10 (UPI) — Lee Thompson Young suffered from bipolar disorder and depression before he fatally shot himself in August, the Los Angeles County coroner said.
The 29-year-old “Rizzoli & Isles” star was taking medication for bipolar disorder and depression when he killed himself. However, no traces of opiates, alcohol, cocaine or other drugs were found in his system, the New York Daily News reported.
Young shot himself in the right temple while sitting on the couch of his North Hollywood apartment. His body was discovered Aug. 19 after he failed to show up for work.
The actor’s specific motive remains unclear, the Daily News said.
The South Carolina native got his big break in acting on the Disney Channel series “The Famous Jett Jackson.”
Please Click HERE to see my products page. There are some bipolar products and also many other products. Make a Difference.
 DIAGNOSTIC DIFFICULTIES IN ASSESSING PSYCHIATRIC COMPLAINTS IN ALCOHOLIC PATIENTS
DIAGNOSTIC DIFFICULTIES IN ASSESSING PSYCHIATRIC COMPLAINTS IN ALCOHOLIC PATIENTS
A Case Example
A 50–year–old man presents to the emergency room complaining: “I’m going to end it all . . . life’s just not worth living.” The clinician elicits an approximate 1–week history of depressed mood, feelings of guilt, and occasional suicidal ideas that have grown in intensity since the man’s wife left him the previous day. The client denies difficulty sleeping, poor concentration, or any changes in his appetite or weight prior to his wife’s departure. He appears unshaven and slightly unkempt, but states that he was able to go to work and function on the job until his wife left. The scent of alcohol is present on the man’s breath. When queried about this, he admits to having “a few drinks to ease the pain” earlier that morning, but does not expand on this theme. He seeks help for his low mood and demoralization, acknowledging later in the interview that “I really don’t want to kill myself; I just want my life back to the way it used to be.”
The above case is a composite of many clinical examples observed across mental health settings each day, illustrating the challenges clinicians face when evaluating psychiatric complaints in alcoholic patients. The questions facing the clinician in this example include:
Is the patient clinically depressed in the sense that he has a major depressive episode requiring aggressive pharmacological and psychosocial treatment?
What role, if any, is alcohol playing in the patient’s complaints?
How does one tease out whether drinking is the cause of the man’s mood problems or the result of them?
If the man’s condition is not a major depression, what is it, what is its likely course, and how can it be treated?
As is usually the case (Anthenelli 1997; Helzer and Przybeck 1988), the patient in this example does not volunteer his alcohol abuse history but comes to the hospital for help with his psychological distress. The acute stressor leading to the distress is his wife’s leaving him; only further probing during the interview uncovers that the reason for the wife’s action is the man’s excessive drinking and the effects it has had on their relationship and family. Thus, a clinician who lacks adequate training in this area or who carries too low a level of suspicion of alcohol’s influence on psychiatric complaints may not consider alcohol misuse as a contributing or causative factor for the patient’s psychological problems.
In general, it is helpful to consider psychiatric complaints observed in the context of heavy drinking as falling into one of three categories—alcohol–related symptoms and signs, alcohol–induced psychiatric syndromes, and independent psychiatric disorders that co–occur with alcoholism. These three categories are discussed in the following sections.
Alcohol–Related Psychiatric Symptoms and Signs
Heavy alcohol use directly affects brain function and alters various brain chemical (i.e., neurotransmitter) and hormonal systems known to be involved in the development of many common mental disorders (e.g., mood and anxiety disorders) (Koob 2000). Thus, it is not surprising that alcoholism can manifest itself in a broad range of psychiatric symptoms and signs. (The term “symptoms” refers to the subjective complaints a patient describes, such as sadness or difficulty concentrating, whereas the term “signs” refers to objective phenomena the clinician directly observes, such as fidgeting or crying.) In fact, such psychiatric complaints often are the first problems for which an alcoholic patient seeks help (Anthenelli and Schuckit 1993; Helzer and Przybeck 1988). The patient’s symptoms and signs may vary in severity depending upon the amounts of alcohol used, how long it was used, and how recently it was used, as well as on the patient’s individual vulnerability to experiencing psychiatric symptoms in the setting of excessive alcohol consumption (Anthenelli and Schuckit 1993; Anthenelli 1997). For example, during acute intoxication, smaller amounts of alcohol may produce euphoria, whereas larger amounts may be associated with more dramatic changes in mood, such as sadness, irritability, and nervousness. Alcohol’s disinhibiting properties may also impair judgment and unleash aggressive, antisocial behaviors that may mimic certain externalizing disorders, such as antisocial personality disorder (ASPD) (Moeller et al. 1998). (Externalizing disorders are discussed in the section “ASPD and Other Externalizing Disorders.”) Psychiatric symptoms and signs also may vary depending on when the patient last used alcohol (i.e., whether he or she is experiencing acute intoxication, acute withdrawal, or protracted withdrawal) and when the assessment of the psychiatric complaints occurs. For instance, an alcohol–dependent patient who appears morbidly depressed when acutely intoxicated may appear anxious and panicky when acutely withdrawing from the drug (Anthenelli and Schuckit 1993; Anthenelli 1997).
In addition to the direct pharmacological effects of alcohol on brain function, psychosocial stressors that commonly occur in heavy–drinking alcoholic patients (e.g., legal, financial, or interpersonal problems) may indirectly contribute to ongoing alcohol–related symptoms, such as sadness, despair, and anxiety (Anthenelli 1997; Anthenelli and Schuckit 1993).
Alcohol–Induced Psychiatric Syndromes
It is clinically useful to distinguish between assorted commonly occurring, alcohol–induced psychiatric symptoms and signs on the one hand and frank alcohol–induced psychiatric syndromes on the other hand. A syndrome generally is defined as a constellation of symptoms and signs that coalesce in a predictable pattern in an individual over a discrete period of time. Such syndromes largely correspond to the sets of diagnostic criteria used for classifying mental disorders throughout the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM–IV) (American Psychiatric Association [APA] 1994) and its successor, the DSM–IV Text Revision (DSM–IV–TR) (APA 2000).
Publication of the DSM–IV marked the first time that clinicians could specifically diagnose several “alcohol–induced disorders” rather than having to lump alcohol–related conditions under the more generic rubric of an “organic mental syndrome” (Anthenelli 1997). Given the broad range of effects heavy drinking may have on psychological function, these alcohol–induced disorders span several categories of mental disorders, including mood, anxiety, psychotic, sleep, sexual, delirious, amnestic, and dementia disorders. According to the DSM–IV, the essential feature of all these alcohol–induced disorders is the presence of prominent and persistent symptoms, which are judged—based on their onset and course as well as on the patient’s history, physical exam, and laboratory findings—to be the result of the direct physiological effects of alcohol. To be classified as alcohol–induced disorders, these conditions also must occur within 4 weeks of the last use of or withdrawal from alcohol and should be of clinical significance beyond what is expected from typical alcohol withdrawal or intoxication (APA 1994).
The diagnostic criteria of the DSM–IV and DSM–IV–TR do not clearly distinguish between alcohol–related psychiatric symptoms and signs and alcohol–induced psychiatric syndromes. Instead, these criteria sets state more broadly that any alcohol–related psychiatric complaint that fits the definition given in the paragraph above and which “warrants independent clinical attention” be labeled an alcohol–induced disorder (APA 1994, 2000). In other words, alcohol–related psychiatric symptoms and signs can be labeled an alcohol–induced psychiatric disorder in DSM–IV or DSM–IV–TR without qualifying as syndromes.
Alcohol–induced psychiatric disorders may initially be indistinguishable from the independent psychiatric disorders they mimic. However, what differentiates these two groups of disorders is that alcohol–induced disorders typically improve on their own within several weeks of abstinence without requiring therapies beyond supportive care (Anthenelli and Schuckit 1993; Anthenelli 1997; Brown et al. 1991, 1995). Thus, the course and prognosis of alcohol–induced psychiatric disorders are different from those of the independent major psychiatric disorders, which are discussed in the next section.
Alcoholism with Comorbid, Independent Psychiatric Disorders
Alcoholism is also associated with several psychiatric disorders that develop independently of the alcoholism and may precede alcohol use and abuse. These independent disorders may make certain vulnerable patients more prone to developing alcohol–related problems (Helzer and Przybeck 1988; Kessler et al. 1997; Schuckit et al. 1997b). One of the most common of these comorbid conditions is ASPD, an axis II personality disorder1 (1The DSM–IV classifies mental disorders along several levels, or axes. In this classification, axis II disorders include personality disorders, such as ASPD or obsessive–compulsive disorder, as well as mental retardation; axis I disorders include all other mental disorders, such as anxiety, eating, mood, psychotic, sleep, and drug–related disorders.) marked by a longstanding pattern of irresponsibility and violating the rights of others that generally predates the problems with alcohol. Axis I disorders commonly associated with alcoholism include bipolar disorder, certain anxiety disorders (e.g., social phobia, panic disorder, and post–traumatic stress disorder [PTSD]), schizophrenia, and major depression (Helzer and Przybeck 1988; Kessler et al. 1997). (Several of these common comorbid disorders are reviewed in detail in other articles of this journal issue.) It is important for clinicians to know which disorders are most likely to coexist with alcoholism so that they may specifically probe for these conditions when evaluating the patient’s complaints.
PSYCHIATRIC DISORDERS COMMONLY ASSOCIATED WITH ALCOHOLISM
Independent Major Depression
Mood disturbances (which frequently are not severe enough to qualify as “disorders”) are arguably the most common psychiatric complaint among treatment–seeking alcoholic patients, affecting upwards of 80 percent of alcoholics at some point in their drinking careers (Brown and Schuckit 1988; Anthenelli and Schuckit 1993). In keeping with the three broad categories described above into which such complaints may fall, mood problems may be characterized as one of the following:
An expected, time–limited consequence of alcohol’s depressant effects on the brain
A more organized constellation of symptoms and signs (i.e., a syndrome) reflecting an alcohol–induced mood disorder with depressive features
An independent major depressive disorder coexisting with or even predating alcoholism.
When one applies these more precise definitional criteria and classifies only those patients as depressive who meet the criteria for a syndrome of a major depressive episode, approximately 30 to 40 percent of alcoholics experience a comorbid depressive disorder (Anthenelli and Schuckit 1993; Schuckit et al. 1997a).
Some controversy exists as to the precise cause–and–effect relationship between depression and alcoholism, with some authors pointing out that depressive episodes frequently predate the onset of alcoholism, especially in women (Kessler et al. 1997; Helzer and Przybeck 1988; Hesselbrock et al. 1985). Several studies found that approximately 60 percent of alcoholics who experience a major depressive episode, especially men, meet the criteria for an alcohol–induced mood disorder with depressive features (Schuckit et al. 1997a; Davidson 1995). The remaining approximately 40 percent of alcoholic women and men who suffer a depressive episode likely have an independent major depressive disorder—that is, they experienced a major depressive episode before the onset of alcoholism or continue to exhibit depressive symptoms and signs even during lengthy periods of abstinence.
In a study of 2,954 alcoholics, Schuckit and colleagues (1997a) found that patients with alcohol–induced depression appear to have different characteristics from patients with independent depressive disorders. For example, compared with patients with alcohol–induced depression, patients with independent depression were more likely to be Caucasian, married, and female; less experienced with other illicit drugs; less often treated for alcoholism; more likely to have a history of a prior suicide attempt; and more likely to have a family history of a major mood disorder.
Bipolar Disorder
According to two major epidemiological surveys conducted in the past 20 years (Helzer and Przybeck 1988; Kessler et al. 1997), bipolar disorder (i.e., mania or manic–depressive illness) is the second–most common axis I disorder associated with alcohol dependence.2 (2 The axis I disorders most commonly associated with alcoholism are other drug use disorders.) Among manic patients, 50–60 percent abuse or become dependent on alcohol or other drugs (AODs) at some point in their illness (Brady and Sonne 1995). Diagnosing bipolar disorder in alcoholic patients can be particularly challenging. Several factors, such as the underreporting of symptoms (particularly symptoms of mania), the complex effects of alcohol on mood states, and common features shared by both illnesses (e.g., excessive involvement in pleasurable activities with high potential for painful consequences) reduce diagnostic accuracy. Bipolar patients are also likely to abuse drugs other than alcohol (e.g., stimulant drugs such as cocaine or methamphetamine), further complicating the diagnosis. As will be described in greater detail later, it can be helpful for an accurate diagnosis to obtain a careful history of the chronological order of both illnesses because approximately 60 percent of patients with both alcoholism and bipolar disorder started using AODs before the onset of affective episodes (Strakowski et al. 2000).
Anxiety Disorders
Overall, anxiety disorders do not seem to occur at much higher rates among alcoholics than among the general population (Schuckit and Hesselbrock 1994). For example, results from the Epidemiologic Catchment Area survey indicated that among patients who met the lifetime diagnosis of alcohol abuse or dependence, 19.4 percent also carried a lifetime diagnosis of any anxiety disorder. This corresponds to only about 1.5 times the rate for anxiety disorders in the general population (Regier et al. 1990; Kranzler 1996). Specific anxiety disorders, such as panic disorder, social phobia, and PTSD, however, appear to have an increased co–occurrence with alcoholism (Schuckit et al. 1997b; Kranzler 1996; Brady et al. 1995).
As with alcohol–induced depression, it is important to differentiate alcohol–induced anxiety from an independent anxiety disorder. This can be achieved by examining the onset and course of the anxiety disorder. Thus, symptoms and signs of alcohol–induced anxiety disorders typically last for days to several weeks, tend to occur secondary to alcohol withdrawal, and typically resolve relatively quickly with abstinence and supportive treatments (Kranzler 1996; Brown et al. 1991). In contrast, independent anxiety disorders are characterized by symptoms that predate the onset of heavy drinking and which persist during extended sobriety.
ASPD and Other Externalizing Disorders
Among the axis II personality disorders, ASPD (and the related conduct disorder, which often occurs during childhood in people who subsequently will develop ASPD) has long been recognized to be closely associated with alcoholism (Lewis et al. 1983). Epidemiologic analyses found that compared with nonalcoholics, alcohol–dependent men are 4–8 times more likely, and alcoholic women are 12–17 times more likely, to have comorbid ASPD (Helzer and Przybeck 1988; Kessler et al. 1997). Thus, approximately 15 to 20 percent of alcoholic men and 10 percent of alcoholic women have comorbid ASPD, compared with 4 percent of men and approximately 0.8 percent of women in the general population. Patients with ASPD are likely to develop alcohol dependence at an earlier age than their nonantisocial counterparts and are also more prone to having other drug use disorders (Cadoret et al. 1984; Anthenelli et al. 1994).
In addition to ASPD, other conditions marked by an externalization of impulsive aggressive behaviors, such as attention deficit hyperactivity disorder (ADHD) (Sullivan and Rudnik–Levin 2001), are also associated with increased risk of alcohol–related problems. (For more information on the relationship between alcoholism and ADHD, see the article by Smith and colleagues, pp. 122–129.)
Please Click HERE to see my products page. There are some bipolar products and also many other products. Make a Difference.
 Bipolar II disorder (pronounced “bipolar two”) is a form of mental illness. Bipolar II is similar to bipolar I disorder, with moods cycling between high and low over time.
Bipolar II disorder (pronounced “bipolar two”) is a form of mental illness. Bipolar II is similar to bipolar I disorder, with moods cycling between high and low over time.
However, in bipolar II disorder, the “up” moods never reach full-on mania. The less-intense elevated moods in bipolar II disorder are called hypomanic episodes, or hypomania.
A person affected by bipolar II disorder has had at least one hypomanic episode in life. Most people with bipolar II disorder also suffer from episodes of depression. This is where the term “manic depression” comes from.
In between episodes of hypomania and depression, many people with bipolar II disorder live normal lives.
Virtually anyone can develop bipolar II disorder. About 2.5% of the U.S. population suffers from some form of bipolar disorder – nearly 6 million people.
Most people are in their teens or early 20s when symptoms of bipolar disorder first start. Nearly everyone with bipolar II disorder develops it before age 50. People with an immediate family member who have bipolar are at higher risk.
During a hypomanic episode, elevated mood can manifest itself as either euphoria (feeling “high”) or as irritability.
Symptoms during hypomanic episodes include:
People experiencing hypomanic episodes are often quite pleasant to be around. They can often seem like the “life of the party” — making jokes, taking an intense interest in other people and activities, and infecting others with their positive mood.
What’s so bad about that, you might ask? Hypomania can also lead to erratic and unhealthy behavior. People in hypomanic episodes might spend money they don’t have, seek out sex with people they normally wouldn’t, and engage in other impulsive or risky behaviors.
Also, the vast majority of people with bipolar II disorder experience significant depressive episodes. These can occur soon after hypomania subsides, or much later. Some people cycle back and forth between hypomania and depression, while others have long periods of normal mood in between episodes.
Untreated, an episode of hypomania can last anywhere from a few days to several months. Most commonly, symptoms continue for a few weeks to a few months.
Depressive episodes in bipolar II disorder are similar to “regular” clinical depression, with depressed mood, loss of pleasure, low energy and activity, feelings of guilt or worthlessness, and thoughts of suicide. Depressive symptoms of bipolar disorder can last weeks, months, or rarely years.
Hypomania often masquerades as happiness and relentless optimism. When hypomania is not causing unhealthy behavior, it often may go unnoticed and therefore remain untreated. This is in contrast to true mania, which by definition causes problems in functioning and requires treatment with medications.
People with bipolar II disorder can benefit from preventive drugs that level out moods over the long term. These prevent the negative consequences of hypomania, and also help to prevent episodes of depression.
Mood Stabilizers
Lithium: This simple metal in pill form is highly effective at controlling mood swings (particularly highs) in bipolar disorder. Lithium has been used for more than 60 years to treat bipolar disorder. Lithium can take weeks to work fully, making it better for long-term treatment than for acute hypomanic episodes. Blood levels of lithium and other laboratory tests (such as kidney and thyroid functioning) must be monitored periodically to avoid side effects.
Depakote: This antiseizure drug also works to level out moods. It has a more rapid onset of action than lithium, and it can also be used for prevention.
Lamictal: This drug is approved by the FDA for the maintenance treatment of adults with bipolar disorder. It has been found to help delay bouts of mood episodes of depression, mania, hypomania (a milder form of mania), and mixed episodes in people being treated with standard therapy.
Some other antiseizure medications, such as Tegretol and Trileptal are also sometimes prescribed.
Antipsychotics
By definition, hypomanic episodes do not involve psychosis and do not interfere with functioning. Antipsychotic drugs, such as Abilify, Risperdal, Seroquel and others, are nevertheless sometimes used in hypomania and some (notably, Seroquel) are used for depression in bipolar II disorder.
Benzodiazepines
This class of drugs includes Xanax, Ativan, and Valium and is commonly referred to as tranquilizers. They are used for short-term control of acute symptoms associated with hypomania such as insomnia or agitation.
Antidepressants
Seroquel and Seroquel XR are the only medications FDA-approved specifically for bipolar II depression. Common antidepressants such as Prozac, Zoloft, and Paxilare also sometimes used in bipolar II depression, and are thought to be less likely to cause or worsen hypomania than is the case in bipolar I disorder. Other medicines sometimes used to treat bipolar II depression include mood stabilizers such as lithium or Depakote, and occasionally Lamictal (although the proven value of Lamictal in bipolar disorder is stronger for preventing relapses than treating acute episodes of bipolar depression). Psychotherapy, such as cognitive-behavioral therapy, may also help.
Because bipolar II disorder typically involves recurrent episodes, continuous and ongoing treatment with medicines is often recommended for relapse prevention.
The causes of bipolar disorder are not well understood. It’s not known if bipolar II disorder can be prevented entirely.
It is possible to prevent some episodes of hypomania or depression, once bipolar disorder has developed. Regular therapy sessions with a psychologist or social worker can stabilize mood, leading to fewer hospitalizations and feeling better overall. Taking medicine on a regular basis also leads to fewer hypomanic or depressive episodes.
People with bipolar I disorder experience true mania — a severe, abnormally elevated mood with erratic behavior. Manic symptoms lead to serious disruptions in life, causing legal or major personal problems.
In bipolar II disorder, the symptoms of elevate mood never reach full-on mania. Hypomania in bipolar II is a milder form of mood elevation. However, the depressive episodes of bipolar II disorder are often longer-lasting and may be even more severe than in bipolar I disorder. Therefore, bipolar II disorder is not simply a “milder” overall form of bipolar disorder.
Please Click HERE to see my products page. There are some bipolar products and also many other products. Make a Difference.
 If you do not have access to any employer-based insurance, do you belong to or could you join any group or association that might offer you a discount on health insurance? Keep in mind that some of these plans may have limited coverage, so make sure you know exactly what you are getting.
If you do not have access to any employer-based insurance, do you belong to or could you join any group or association that might offer you a discount on health insurance? Keep in mind that some of these plans may have limited coverage, so make sure you know exactly what you are getting.
Information for Wisconsin about the Health Insurance Marketplace under the Affordable Care Act is available from HealthCare.gov. The Health Insurance Marketplace is a new way to get coverage that meets your needs. Starting October 1, 2013, you can come to HealthCare.gov to fill out an application and see your plan choices. In the meantime, this site will help you get ready. More information from HealthCare.gov.
There are several types of health spending accounts on the market today. Health Savings Accounts (HSAs) are one type of health spending account.Information on HSAs is available.
Finding insurance as an individual means special concerns, including generally higher costs and less complete coverage. In addition, your health can affect the type of coverage you can get. Before you can buy an individual policy you must give the insurance company information about your health. This process is called medical underwriting.
As the cost of health care rises, health insurance scams are becoming more common. Watch out for unlicensed insurers that offer cheap coverage but then refuse to pay claims. Also be wary of so-called “discount health plans” that are not really insurance at all, but advertise in ways that make it sound as if they are. When in doubt, contact Wisconsin’s Office of the Commissioner of Insurance at (608) 266-3585 (from Madison) or (800) 236-8517 to confirm that you are working with a licensed insurer. Remember, if it sounds too good to be true, it probably is.
Tips on buying individual health coverage are provided by Insure.com.
If you are trying to decide whether to work with an insurance agent or to contact the insurance companies directly, keep in mind that some insurance companies only work through agents/brokers while some agents only offer insurance for one or two insurance companies.
There are several commercial tools such as Insure.com, eHealthinsurance.com, and healthcareshopper.com available on the Internet that provide instant insurance quotes. Before you use this approach, consider the precautions (PDF, 27 KB) suggested by the National Association of Insurance Commissioners.
Catherine Zeta-Jones: Her History of Mental Illness
 Catherine Zeta-Jones is currently in a treatment center receiving help to control her bipolar II disorder, an ongoing struggle she has been candid about over the years.
Catherine Zeta-Jones is currently in a treatment center receiving help to control her bipolar II disorder, an ongoing struggle she has been candid about over the years.
The 43-year-old Oscar-winning actress went public with her mental health battle in 2011. After her husband, Michael Douglas, received the good news that his Stage IV throat cancer was gone that January, she couldn’t fight a lingering depression. In April of that year, she checked into a mental health facility in Connecticut and during her five-day stay there, she was diagnosed with bipolar II disorder, a mental illness marked by prolonged periods of depression alternating with episodes of mild mania.
“This is a disorder that affects millions of people and I am one of them,” the actress, told People at the time. “If my revelation of having bipolar II has encouraged one person to seek help, then it is worth it. There is no need to suffer silently and there is no shame in seeking help.”
Zeta-Jones first began suffering from anxiety several years earlier — around the time she was filming 2004’s “Ocean’s Twelve” and she was also dealing with a stalker. However, she tried to fight it, telling Britain’s Sunday Times in 2010, “Being negative isn’t good for my personality. I don’t just bring myself down; I bring everyone around me down. It’s like a dark cloud. ‘Uh-oh, here we go,’ and I have to snap out of it.”
While Zeta-Jones seemed to be comfortable going public with the disorder, in December 2012 she seemed a bit less so.
“You know what, I’m sick of talking about it because I never wanted to be the poster child for this,” Zeta-Jones told “Good Morning America.” “I never wanted this to come out publicly. It came out. And so I dealt with it in the best way I could and that was just say, ‘Look, hey, I’m bipolar.’”
“Everyone has things going on and we deal with them the best we can,” she continued. “We can’t jump from the rooftops shouting, you know, about, ‘I have this, look at me, victim.’ No. We all have issues in life and I’m really happy that I have great friends, great support, and that’s all I can do.”
And she has her support system in place now that she’s in treatment again. It was announced on Monday — after her husband attended the White House Correspondents’ Dinner by himself — that she is again seeking help in an in-patient facility.
“Catherine has proactively checked into a health care facility,” a rep for the actress said in a statement Monday night. “Previously Catherine has said that she is committed to periodic care in order to manage her health in an optimum manner.”
HERE YOU CAN FIND PRODUCTS ABOUT HEALTHY LIVING & BIPOLAR DISORDER!!
SAN DIEGO, Calif. – Like most severely mentally ill patients, 23-year-old Daniel Padilla doesn’t see himself as that.
The insurance companies that cover him – Medi-Cal (California’s name for Medicaid, the federal-state-funded insurance for low-income and disabled people) and United Health Insurance — don’t see the schizophrenia he was diagnosed with at age 19, as deserving the same benefits as someone with a medical condition.
His father, Benito, must go after the insurers month after month to get them to pay Padilla’s psychiatrist to keep his schizophrenia under control.
“The insurers approve three visits and then they put you through hell,” asserted San Diego-based psychiatrist Dr. Rodrigo A. Muñoz, who has been treating Padilla all along.
“Insurers discriminate against people who are mentally ill,” Muñoz said.
But that’s all going to change soon. When the historic Affordable Care Act fully unrolls on Jan. 1, 2014, it will require insurers to offer mental health care benefits equal to physical health benefits. In other words, a disorder in the brain will be treated no differently than one in the kidney, Muñoz said.
Not just people with mental disorders, but those with substance use disorders have encountered penny-pinching annual and lifetime caps on coverage, higher deductibles, or simply no coverage at all.
Federal Parity Law
The blatantly discriminatory practices by health insurance companies prompted Congress in 2008 to pass the Mental Health Parity and Addiction Equity Act (MHPAEA), which mandated that psychiatric illness be covered just the same as other medical illnesses. It required insurers to offer the same annual and lifetime dollar limits for mental health care as for medical and surgical care.
But the law applies only to larger employers – those with 50 or more workers – that offered a health plan that covered mental health and substance abuse. Smaller employers, as well as people who buy their own insurance, are excluded from the benefits of the law.
“Smaller employers have resisted changing the law, saying they will go broke” if they had to include mental health coverage in their health care plans, Muñoz pointed out.
The ACA has extended the MHPAEA provisions to state insurance exchanges, known as Covered California in this state. This would require policies purchased by smaller employers and individuals through the exchange, as well as those purchased outside of it, to be MHPAEA-compliant.
Had the MHPAEA mandated universal psychiatric benefits when it was created, insurers like Padilla’s would not have been able to discriminate between the treatment of psychiatric and non-psychiatric medical illnesses, he said.

Only a Fraction of the Mentally Ill Get Treatment
Dr. Clayton Chau, who practices psychiatry in Orange County, Calif., said that because of the discrimination factor, poor access to care and inadequate insurance coverage, only a fraction of those with mental illness get treatment.
A report by the Surgeon General indicates that one in four Americans has a diagnosable mental illness at any given time. National and international studies show that 1 percent of the general population has schizophrenia, an illness that is treatable, though not curable. Surveys, including those done by the National Institutes of Mental Health, show that only about 50 percent of Americans seek psychiatric treatment.
According to Randall Hagar, director of government relations with the California Psychiatric Association, a state mental health parity bill signed by Gov. Davis in 2000 required insurers to cover the diagnosis and treatment of a range of mental illnesses under “the same terms and conditions applied to other medical conditions.” The intent of the law was to eliminate the disparity in co-pays and higher deductibles.
In the opinion of many advocates, Hagar observed, the law i
s
“routinely violated by plans and insurers, and enforcement is generally weak.”
That prompted Sen. Jim Beall, D-Campbell, to try five times to give more teeth to federal and state mental health parity laws. Beall’s first four bills were
vetoed by Gov. Schwarzenegger, and his most recent bill (SB22) didn’t even make it out of committee
What the Health Care Law Will Do
Under the ACA, aka Obamacare, health insurers are forbidden from excluding people with pre-existing illness from medical coverage. By definition, Americans with a mental illness have a pre-existing disorder, and up until now, private health insurers have denied with impunity coverage to those with pre-existing conditions.
California has added a mental health component to its expanded Medi-Cal program, under ACA, to ensure that its Medi-Cal population with mental disabilities receives more comprehensive mental health benefits, starting Jan. 1, 2014.
The current mental health component of Medi-Cal “is limited in terms of the number of providers and the number of services” it offers, Chau said.
Older people with mental illness will also benefit from the ACA because the law will close the notorious “donut hole,” allowing the Medicare population to not have a break in medication.
Padilla, who’s currently working for his GED, has been able to stay on his father’s insurance because of his age. A provision in the ACA allows children under 26 to remain on a parent’s insurance plan.
Muñoz is relieved that the ACA will help patients like Padilla access the care they so badly need. The removal of lifetime caps by insurance companies will enable mentally ill patients to access care before turning to suicidal thoughts, becoming violent or ending up homeless, he said.
.
 Before the Affordable Care Act was passed in 2010, one’s right to appeal decisions made by their health plan varied depending on which state they lived in, their type of health insurance, and whether they bought their own insurance or were covered through a job. In some states, when people disagreed with their health plan’s decision, they could appeal that decision to experts outside of their health plan, and in other states, they had no appeal rights.
Before the Affordable Care Act was passed in 2010, one’s right to appeal decisions made by their health plan varied depending on which state they lived in, their type of health insurance, and whether they bought their own insurance or were covered through a job. In some states, when people disagreed with their health plan’s decision, they could appeal that decision to experts outside of their health plan, and in other states, they had no appeal rights.
The federal healthcare reform law assures the same level of appeal rights to everyone with private health insurance, if they buy their own policy or get coverage through a group plan provided from their job. For new health plans that you or your employer purchase after March 23, 2010, if you disagree with your plan’s refusal to pay for care, the plan will have to review its decision. And if you still are not satisfied, you will have the right to appeal that decision to an independent reviewer who is outside of the health plan. (If you are in a health plan that you or your employer purchased before March 23, 2010, check with your state insurance department, your employer, and your health plan to find out whether you have similar appeal rights.)
You can appeal a plan’s decision not to pay for a benefit, or to reduce or end a covered service, when the plan says any of the following: (1) the care is not medically necessary or appropriate, (2) you are not eligible for the health plan or benefit, (3) you have a pre-existing condition, or (4) the care is experimental or investigational. If the plan has told you any of these things and you do not agree, you can appeal. You can also appeal when the plan rescinds your coverage (cancels your coverage retroactively). The plan must give you a notice when it denies payment or rescinds your coverage that explains both their reason, how you can appeal, and any applicable deadlines.
The following are some examples of other health plan determinations or rules you can appeal:
If you believe the service, device, treatment, or medication in question should have been covered by your plan, you can and should appeal. Many people do not pursue their appeal rights because they don’t believe they can win. But if you are dissatisfied with the outcome of a claim for any reason, you have nothing to lose by taking advantage of your right to request a re-consideration of the original claim. Start by re-examining your plan manual to make sure what you presumed would be covered really is. It is not unusual for people to discover that a medical service or treatment is not covered by their policy. If something is specifically excluded from the policy, chances of winning coverage for it on appeal are slim to none. But if the policy does not mention the specific treatment in question or the coverage is unclear or framed in terms of ‘medical necessity’, it is to your advantage to try the appeals process.
Carefully review the explanation of benefits (EOB) form (official response to your claim) they sent you. Make sure you understand the reason you have been denied coverage or why you are not being reimbursed more money. These explanations often appear as codes with explanatory notes at the bottom or on the back. Is there a simple explanation, such as, the claim is a duplicate? Is there a mistake in the billing code, patient identification number, date of service or other? If all this information seems in order, your next step is to understand your plan’s Appeal Procedures. Look in your manual (sometimes under “Grievances and Appeals”). Follow these procedures carefully, especially the deadlines, as well as these basic guidelines:
Be sure to discuss your insurer’s denial, or other coverage issue you are appealing with your physician (or other relevant health care provider) to solicit his/her active support. If the dispute is over the necessity or value of a medical treatment, your physician’s support in the form of a letter including studies supporting the benefit of the treatment in question could be invaluable. Provide copies of your appeal letter to your physician (or other provider) for their records. Make sure you do not duplicate efforts. If the dispute is over the medical necessity or value or a medical treatment, your physician is a powerful ally. A physician’s letter that refers to scientific studies supporting the benefit of the treatment in question could be invaluable. The National MS Society provides model letters of appeal for a variety of therapies in an appeal letters toolkit for physicians to help you both with the process.
 When done, print the bipolar depression test (bipolar depression quiz) and share the results with your doctor.
When done, print the bipolar depression test (bipolar depression quiz) and share the results with your doctor.
1. Do you experience extreme mood changes – going from extremely happy to extremely sad?
Answer:
If you checked yes or sometimes to bipolar depression test question 1, it’s possible you exhibit the traditional signs of bipolar disorder.
2. Do you have anyone in your family (include all relatives) who has been diagnosed with bipolar disorder?
Answer:
If you check yes to question 2, bipolar disorder does have a genetic component and research shows bipolar disorder tends to run in families.
3. Do you experience periods where you feel any of the following (check all that apply):
Persistent sad, anxious or “empty” feelings
Feelings of hopelessness and/or pessimism
Feelings of guilt, worthlessness and/or helplessness
Irritability, restlessness
Loss of interest in activities or hobbies once pleasurable, including sex
Fatigue and decreased energy
Difficulty concentrating, remembering details and making decisions
Insomnia, early–morning wakefulness, or excessive sleeping
Overeating, or appetite loss
Thoughts of suicide, suicide attempts
Persistent aches or pains, headaches, cramps or digestive problems that do not ease even with treatment
Answer:
Question 3 measures the traditional symptoms of major depression. If you’ve experienced five (or more) of those symptoms during the same 2-week period and at least one of the symptoms is either: (1) depressed mood or (2) loss of interest or pleasure, this is an indication you may have Major Depressive Disorder.
4. Have you ever experienced any of these symptoms for a period of at least one week?
Elevated mood
Euphoria
Hyperactivity
Excitement
Overconfidence
Grandiosity
Extravagance
Spending sprees
Recklessness
Delusions of grandeur
Talking a lot
Rapid speech
Rapid movements
Reduced need for sleep
Increased appetite
Excessive exercising
Increased libido
Increased use of alcohol
Distractedness
Aggression
Excessive laughter
Anger
Answer:
Question 4 of the bipolar depression test measures the symptoms of mania and hypomania. Remember, the difference between bipolar depression vs depression is the person must have also experienced the symptoms of bipolar mania or hypomania. If you checked off symptoms in this question and question 3, please discuss the possibility that you might have bipolar depression with your doctor or mental health professional.
Reference: http://www.healthyplace.com
There are significant differences between these two forms of bipolar disorder. The information below is taken mostly from the fourth edition of theDiagnostic and Statistical Manual of Mental Disorders(or DSM-IV). It should be noted that possible major changes are proposed for the upcoming fifth edition; however, some of the important proposed changes as currently written conflict with each other, and thus I am relying on the fourth edition at this time.
Note: Because the terms bipolar I and II are used interchangeably with bipolar 1 and 2 (bipolar II is even often mistyped as bipolar 11!), I have used those terms interchangeably in this article.
Here’s a summary of the most important differences between bipolar I and II.
The main difference between mania and hypomania is a matter of severity. In the hypomania of bipolar 2, a person has a sustained mood that is elevated (heightened), expansive (grand, superior) or irritable. This mood has to be noticeably different from his or her normal mood when not depressed. In mania, that mood is abnormally different, and is also combined with increased activity or energy that is also abnormal.
For example, Hank, when he has hypomanic episodes, is exceptionally cheerful, needs only three hours sleep instead of his usual seven, spends more money than he safely should and speaks far more rapidly than usual, along with other symptoms of hypomania. This behavior isnoticeably different from his own stable mood, yet there are cheerful people who need little sleep, spend a lot and talk fast who don’t have bipolar disorder, so it’s not considered abnormal.
On the other hand, Hank’s friend Robert, who has manic episodes, is out-of-control happy, even during serious events (he burst out laughing disruptively during a funeral). He ran around outside at midnight shouting how much he loved all his neighbors (along with other symptoms of mania). This is abnormal behavior for anyone.
One or more of the following conditions has to exist in mania but can’t be present in hypomania:
Robert firmly believes he is the mayor of his town and introduces himself to people as such, telling them about grandiose and sometimes bizarre plans he has for making improvements to services and infrastructure. If Hank had a similar delusion, his diagnosis would be bipolar I rather than bipolar II. The presence of psychosis automatically rules out hypomania.
Robert missed an important business meeting because of a spur-of-the-moment decision to take flying lessons. Hank may be longing to take flying lessons while hypomanic, but if he does, he takes them at a reasonable time when he has no other obligations.
During an irritable manic episode, Robert began throwing crockery, silverware, pots and pans at his wife because he wasn’t satisfied with that night’s dinner. He was subsequently hospitalized because he had become a danger to others. Hank’s hypomania does not escalate to such an extreme extent.
Although the presence of psychotic symptoms is one of the things that differentiates bipolar I mania from bipolar II hypomania, someone with bipolar II may experience hallucinations or delusions during depressive episodes without the diagnosis changing to bipolar I.
 Recently, a friend asked me, “Julie, why don’t you write a book about bipolar disorder and relationships?” “I already did that with my first book for couples where one person has bipolar,” I replied. “I don’t mean couples, Julie!” he exclaimed. “I mean friendships. I can’t seem to keep any friends.”
Recently, a friend asked me, “Julie, why don’t you write a book about bipolar disorder and relationships?” “I already did that with my first book for couples where one person has bipolar,” I replied. “I don’t mean couples, Julie!” he exclaimed. “I mean friendships. I can’t seem to keep any friends.”
I know what my friend—a man in his late 30s who struggles with bipolar disorder—meant by this statement. Like me, he wanted good relationships, but often found that bipolar got in the way. In the years after I was finally diagnosed with bipolar in1995, I managed to lose almost all my friends because of my neediness, irritation, paranoia, medication side effects, and more. In 2001, I hit rock bottom when I received a letter from my best friend (I’ll call her “Melissa”)that changed my life forever. While it was terribly hard to read, this letter ,in fact, saved my future relationships.
Melissa and I had been friends since high school; I was always the aggressive force in the relationship. As my illness got progressively worse, I became weak while she became strong. She started sticking up for herself; I, on the other hand, began to sink into a hole of depression that seemed inescapable. I called Melissa constantly and complained about my life. When she didn’t respond the way I wanted, I became paranoid and angry, telling her she wasn’t a good friend.
An unwelcome look at ‘relationship killers’
Looking back on it now, I had become prey to the typical bipolar relationship killers—neediness, selfishness, and paranoia. One day, my friend, in a five-page, single-spaced letter, made it clear that she couldn’t take it anymore:
It seems to be a continual problem with us that you think I don’t spend enough time with you. What am I to do? I go long stretches of time without seeing lots of people, and they just don’t seem to have a problem with it. They are busy, too. They have lives. I guess I’m just tired after all these years of feeling like I have to continually defend myself that I don’t give you what you need. I wish you could accept what I give and not seem to continually feel that I’m not giving enough.
I cried and cried when I read Melissa’s letter. How had this happened? I was indignant, angry, and sad—I felt misunderstood and attacked. Didn’t she understand how terrible bipolar is? How could she be so insensitive? I had been the popular one in high school and used to have so many friends. I was mortified as I read on:
Julie, you are such a wonderful person. I could list 50 positive things about you. But I can’t be the primary support person in your life that you seem to continually want me to be. I don’t have anything left. I’m 36 and I don’t want to be the caretaker I was in my teens and 20s. I want to care for me. That doesn’t mean that I’m a bad friend or a bad person.
Overcoming the ‘bipolar trap’
At the time, I overlooked the words, Julie, you are a wonderful person. All I saw was the criticism. Iwas utterly unaware of the “bipolar trap”—allowing my mood swings to determine my behavior and in the process losing all reasoning.
Indeed, because my depression made me needy, I excessively looked to others for help. Selfishly, I couldn’t focus on the lives of my friends—my despair was all-consuming. Finally, my paranoia became so intense—I couldn’t stop myself from sending long, rambling emails about how people didn’t really care for me.
The final blow came toward the end of Melissa’s letter:
I want you to have fun with my friends. One friend liked you a lot, but she was a bit concerned with the slew of illnesses you described. I know you want to be honest about your illness, but you also have to realize that [your fulsome descriptions] can scare people off on a first meeting. Sometimes I want to include you with things I do with friends, [but] they would prefer not to.
As I read this passage, I realized that few people really wanted my company. Honestly, I had no idea that bipolar’s mood swings could do this to a person—I was still blaming others for my unhappiness.
Concluding her letter, Melissa said that while she cared about me, she could no longer be friends. I replied with a long, miserable email about how she didn’t understand how hard life was for me—she was insensitive!
Eventually, most of my friends left me. Because my self-treatment plan was then at a beginning stage, I hadn’t made the connection between bipolar’s mood swings and my own behavior.
After reading Melissa’s letter over and over and weighing my options, I had a moment of clarity that I can vividly recall: I could stay as I was—miserable and friendless—or I could take advantage of this amazing gift my friend had unknowingly handed me. With these reflections, I felt my hurt and my anger slip away. To get better, I would have to change every negative behavior Melissa had described. I had no idea how I was going to do this—the problem appeared insurmountable. Still, I made the important connection that if I could somehow control my bipolar disorder, I would become a better friend. This meant finding a way to manage my symptoms. In this way, I could manage my behavior toward potential friends even when I was experiencing the mood swings. Furthermore, I realized that myself-treatment plan simply wasn’t working at that point. I needed to make a change if I was going to get better.
Turning things around
Confronting my shortcomings was one of the most painful things I’ve ever done. It made me realize that there was nothing wrong with my friends; rather, there was something wrong with me. So I let go of my pride and got to work—I learned to manage the illness and my emotions to the point that I started to become a better friend.
It took me many years to truly change, but I kept going. I stopped talking so much and started listening.
I consciously tried not to monopolize the conversation with my health worries. By using the self-treatment plan that I developed and now discuss in my books, I began to recognize the signs of these relationship killers and to limit their occurrence.
As I began to better manage the illness, I saw the huge connection between the random emotions caused by untreated bipolar disorder and the real me—the good me—beneath all the symptoms. I taught myself to live by the new code I had created and not according to this horrible illness.
Now—seven years after receiving this letter—I’m surrounded by friends whom I care about deeply. They often compliment me on my friendship skills. Sometimes I tell them about this letter, explaining that it’s still a struggle for me to be a good friend. And while I have certainly wrecked a few relationships over the past few years, I know that I have come a long way.
Unfortunately, Melissa and I stopped seeing each other in 2001. She has no idea that she changed my life with her compassionate, kind, and truthful letter. Perhaps I should send her this column and let her know she is one of the main reasons I’m now able to write books that help others become better friends.
—–
Julie A. Fast, along with John Preston, Psy D, is co-author of Get It Done When You’re Depressed, Loving Someone with Bipolar Disorder: Understanding and Helping Your Partner, and Take Charge of Bipolar Disorder: A 4-Step Plan for You and Your Loved Ones to Manage the Illness and Create Lasting Stability.
–SIDEBAR–
Tips for being a better friend
Listen more than you talk.
Limit talk about your health problems.
Stop complaining and start changing.
Don’t send email or make phone calls when you’re feeling sick and needy. It will never go well.
Read about the “bipolar conversation” I discuss in all my books.
Always ask yourself, is this the real me or the bipolar me? Then make sure the “real you” is in control when you see your friends.
Give yourself time to change. You can become a superb friend in less than a year!
reference: http://www.bphope.com
True Story about Bipolar Disorder & Marriage
Douglas is said to be in Sardinia on his own, while Zeta Jones remains in New York with their two children.
Zeta Jones’s publicist told The Daily Telegraph: “Catherine and Michael are taking some time apart to evaluate and work on their marriage. There will be no further comment.”
The couple, who married in 2000, were last pictured together on the red carpet in April.
Neither of the pair is said to have filed for divorce or moved towards a legal separation.
But they have been seen to spend time apart since Douglas, 68, returned from the Cannes Film Festival in France in May. His wife is believed to be staying in New York with their children Dylan, 13, and Carys, 10 while he is on holiday alone in Sardinia.
A source told People magazine that difficulties over the last three years – including Douglas’s battle with cancer and his wife’s struggle with bipolar II disorder – had “taken a toll on their marriage.”
Zeta Jones has previously spoken about bipolar II disorder, a milder version of the illness characterised by mood swings and episodes of depression. She had treatment for the condition in 2011 and earlier this year.
Despite reports that Zeta Jones was preparing for a £300m divorce against her husband, according to Star magazine, representatives for Douglas have denied the couple have separated.
The Hollywood actor recently spoke about his divorce from his first wife Diandra, which he admitted should have ended sooner. He said: “I know I’m going to get into trouble here. I have nothing against her and in fact I’m very fond of my first wife. But we should have ended that marriage eight or 10 years earlier.”
Please Click HERE to see my products page. There are some bipolar products and also many other products. Make a Difference.
Symptoms of Childhood Bipolar Disorder
 Childhood bipolar disorder, also known as pediatric bipolar disorder, is a form of bipolar disorder that occurs in children. While its existence is still a matter of some academic debate and disagreement, there is a growing body of evidence that suggests that bipolar disorder can exist in children.
Childhood bipolar disorder, also known as pediatric bipolar disorder, is a form of bipolar disorder that occurs in children. While its existence is still a matter of some academic debate and disagreement, there is a growing body of evidence that suggests that bipolar disorder can exist in children.
Unlike most adults who have bipolar disorder, however, children who have pediatric bipolar disorder are characterized by abrupt mood swings, periods of hyperactivity followed by lethargy, intense temper tantrums, frustration and defiant behavior. This rapid and severe cycling between moods may produce a type of chronic irritability with few clear periods of peace between episodes.
Because the current diagnostic manual of mental disorders doesn’t recognize childhood bipolar disorder, there is no official symptom criteria. However, researchers have used criteria similar to that of adult bipolar disorder, requiring a child or teen to meet at least four or more of the following:
Keep in mind that many of these behaviors, in and of themselves, are not indicative of a possible disorder and are characteristic of normal childhood development. For instance, separation anxiety, by itself, is a normal fear of being separated from one or both of the parents (for instance, attending the first day of first grade or if the parents want to go out for a night).
Childhood bipolar disorder is characterized by many of these symptoms, taken together, and marked by rapid mood swings and hyperactivity. These symptoms must also cause significant distress in the child or teen, occur in more than just one setting (e.g., at school and at home), and last for at least 2 weeks.
Because the existing diagnostic manual doesn’t recognize pediatric bipolar disorder, and there is still debate within the professional community about the validity of this diagnosis, insurance companies may not reimburse for treatment of this disorder. In addition, some professionals may not recognize the disorder and misdiagnose the child or teen with attention deficit disorder or depression.
 Bipolar I disorder (pronounced “bipolar one” and also known as manic-depressive disorder or manic depression) is a form of mental illness. A person affected by bipolar I disorder has had at least one manic episode in his or her life. A manic episode is a period of abnormally elevated mood, accompanied by abnormal behavior that disrupts life.
Bipolar I disorder (pronounced “bipolar one” and also known as manic-depressive disorder or manic depression) is a form of mental illness. A person affected by bipolar I disorder has had at least one manic episode in his or her life. A manic episode is a period of abnormally elevated mood, accompanied by abnormal behavior that disrupts life.
Most people with bipolar I disorder also suffer from episodes of depression. Often, there is a pattern of cycling between mania and depression. This is where the term “manic depression” comes from. In between episodes of mania and depression, many people with bipolar I disorder can live normal lives.
Virtually anyone can develop bipolar I disorder. About 2.5% of the U.S. population suffers from bipolar disorder — almost 6 million people.
Most people are in their teens or early 20s when symptoms of bipolar disorder first appear. Nearly everyone with bipolar I disorder develops it before age 50. People with an immediate family member who has bipolar are at higher risk.
During a manic episode in someone with bipolar disorder, elevated mood can manifest itself as either euphoria (feeling “high”) or as irritability.
Abnormal behavior during manic episodes includes:
People in manic episodes may spend money far beyond their means, have sex with people they wouldn’t otherwise, or pursue grandiose, unrealistic plans. In severe manic episodes, a person loses touch with reality. They may become delusional and behave bizarrely.
Untreated, an episode of mania can last anywhere from a few days to several months. Most commonly, symptoms continue for a few weeks to a few months. Depression may follow shortly after, or not appear for weeks or months.
Many people with bipolar I disorder experience long periods without symptoms in between episodes. A minority has rapid-cycling symptoms of mania and depression, in which they may have distinct periods of mania or depression four or more times within a year. People can also have mixed episodes, in which manic and depressive symptoms occur simultaneously, or may alternate from one pole to the other within the same day.
Depressive episodes in bipolar disorder are similar to “regular” clinical depression, with depressed mood, loss of pleasure, low energy and activity, feelings of guilt or worthlessness, and thoughts of suicide. Depressive symptoms of bipolar disorder can last weeks or months, but rarely longer than one year.
Manic episodes in bipolar I disorder require treatment with drugs, such as mood stabilizers and antipsychotics, and sometimes sedative-hypnotics (benzodiazepines such as Ativan or Klonopin).

Mood Stabilizers
Lithium: This simple metal in pill form is especially effective at controlling mania that involves classical euphoria rather than mixtures of mania and depression simultaneously. Lithium has been used for more than 60 years to treat bipolar disorder. Lithium can take weeks to work fully, making it better for maintenance treatment than for sudden manic episodes. Blood levels of lithium as well as tests to measure kidney functioning must be monitored to avoid side effects.
Depakote: This antiseizure medication also works to level out moods. It has a more rapid onset of action, often making it more effective for an acute episode of mania than lithium. It is also often used “off label” for prevention of new episodes. Only mood stabilizers that can be used with the loading dose method — beginning at a very high dose — allow the possibility of significant improvement in mood as early as four to five days.
Some other antiseizure drugs, notably Tegretol and Lamictal, can have value in treating or preventing manias or depressions. Other antiseizure medicines that are less well-established for the treatment of bipolar disorder, include Trileptal, Neurontin, and Topamax.
Antipsychotics
For severe manic episodes, traditional antipsychotics (such as Haldol or Thorazine) as well as newer antipsychotic drugs — also called atypical antipsychotics — may be necessary. Abilify, Risperdal, Saphris, Seroquel, Geodon, and Zyprexa are often used, and many other drugs are available. The antipsychotic Latuda is approved for use — either alone or with lithium or Depakote — in cases of bipolar I depression.Antipsychotic medicines are also sometimes used for preventive treatment.
Benzodiazepines
This class of drugs includes Xanax, Ativan, and Valium and is commonly referred to as tranquilizers. They are sometimes used for short-term control of acute symptoms associated with mania such as agitation or insomnia, but they do not treat core mood symptoms such as euphoria or depression.
Antidepressants
Common antidepressants such as Prozac, Zoloft, and Paxil have not been shown to be as effective for treating depression in bipolar disorder as in unipolar depression. In a small percentage of people, they can also set off or worsen a manic episode in a person with bipolar disorder. For these reasons, the first-line treatments for depression in bipolar disorder involve medicines that have been shown to have antidepressant properties but also no known risk for causing or worsening mania. The two FDA-approved treatments for bipolar depression are Seroquel or Seroquel XR and Symbyax (olanzapine-fluoxetine) combination. Other mood-stabilizing treatments that are sometimes recommended for treating acute bipolar depression include lithium, Depakote, and Lamictal (although none of these medicines is FDA-approved specifically for bipolar depression). If these fail, after a few weeks a traditional antidepressant or other medicine may sometimes be added. Psychotherapy, such as cognitive-behavioral therapy, may also help.
People with bipolar I disorder (mania or depression) have a high risk for recurrences and usually are advised to take medicines on a continuous basis for prevention.
Electroconvulsive Therapy (ECT)
Despite its scary reputation, electroconvulsive therapy (ECT) is an effective treatment for manic symptoms. ECT is seldom used to treat bipolar I disorder, but can be helpful if medicines fail or can’t be used.
The causes of bipolar disorder are not well understood. It’s not known if bipolar I disorder can be prevented entirely.
It is possible to prevent some episodes of mania or depression once bipolar disorder has developed. Regular therapy sessions with a psychologist or social worker can help people to identify factors that can destabilize mood (such as sleep deprivation, drug or alcohol abuse, and poor stress management), leading to fewer hospitalizations and feeling better overall. Taking medicine on a regular basis can help to prevent future manic or depressive episodes.
People with bipolar I disorder experience true mania — the often severe abnormally elevated mood and behavior described above. These manic symptoms can lead to serious disruptions in life (for example, spending the family fortune, or having an unintended pregnancy).
In bipolar II disorder, the symptoms of elevated mood never reach full-on mania. They often pass for extreme cheerfulness, even making someone a lot of fun to be around — the “life of the party.” This less-severe mania is called hypomania. Not so bad, you might think — except bipolar II also features episodes of significant depression.
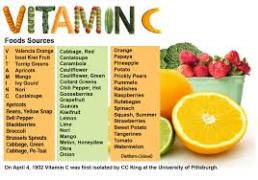 I have looked at bipolar and what I found interesting was the study that says Vitamin C may help. The way I read the study, EDTA is not good for those who are Manic Bi-Polar and Vitamin C is beneficial. From the study, If I was bi-polar, I would stay away from foods with vanadium such as breads and cereal with wheat, radishes, black pepper, mushrooms, soy products, shellfish, shark, tuna, commercially raised chicken and turkey (they are given meal with high levels of vandium), vinegar, pickles, reduce or eliminate refined sugar, corn, olive oils, sunflower seeds, oats, rice, carrots, green beans, lettuce, cabbage, parsley, and dill seed. Foods low in vanadium include fresh fruits and vegetables. I would subtitute my foods high in vandium with more fresh fruits and vegetables(other than those listed) rather than eating wheat based foods like pasta, pizza, sandwiches etc… I make a fruit smoothie every morning and juice fruits and veggies.
I have looked at bipolar and what I found interesting was the study that says Vitamin C may help. The way I read the study, EDTA is not good for those who are Manic Bi-Polar and Vitamin C is beneficial. From the study, If I was bi-polar, I would stay away from foods with vanadium such as breads and cereal with wheat, radishes, black pepper, mushrooms, soy products, shellfish, shark, tuna, commercially raised chicken and turkey (they are given meal with high levels of vandium), vinegar, pickles, reduce or eliminate refined sugar, corn, olive oils, sunflower seeds, oats, rice, carrots, green beans, lettuce, cabbage, parsley, and dill seed. Foods low in vanadium include fresh fruits and vegetables. I would subtitute my foods high in vandium with more fresh fruits and vegetables(other than those listed) rather than eating wheat based foods like pasta, pizza, sandwiches etc… I make a fruit smoothie every morning and juice fruits and veggies.
Vitamin C helps the body to reduce its load of vanadium and this has been studied for its possible role in treatment of bipolar disorder.35 A double-blind trial found that both manic and depressed bipolar patients were significantly improved after one-time administration of 3 grams of vitamin C, compared with a placebo.36 The same study found that both manic and depressed patients did better on a reduced-vanadium diet compared to a normal diet. Another double-blind study reported that 4 grams per day of vitamin C in combination with a drug known as EDTA (which also helps remove elements such as vanadium from the body) was helpful to depressed bipolar patients but not to those experiencing mania.37 Until more is known, people with bipolar illness should avoid supplements containing vanadium and consider supplementing with vitamin C.
http://www.vitacost.com/science/hn/Concern/Bipolar_Disorder.htm
I would also suggest going to the Vitamin C forum if you have questions about Vitamin.
From Owen’s advice to others, I would take high doses of Vitamin C but make sure to use sodium ascorbate crystals for the best results. I would start off slow 500mg but work my way up to 4,000 mg per day.
http://www.curezone.com/forums/f.asp?f=400&p=9
I have looked at bipolar and what I found interesting was the study that says Vitamin C may help. The way I read the study, EDTA is not good for those who are Manic Bi-Polar and Vitamin C is beneficial. From the study, If I was bi-polar, I would stay away from foods with vanadium such as breads and cereal with wheat, radishes, black pepper, mushrooms, soy products, shellfish, shark, tuna, commercially raised chicken and turkey (they are given meal with high levels of vandium), vinegar, pickles, reduce or eliminate refined sugar, corn, olive oils, sunflower seeds, oats, rice, carrots, green beans, lettuce, cabbage, parsley, and dill seed. Foods low in vanadium include fresh fruits and vegetables. I would subtitute my foods high in vandium with more fresh fruits and vegetables(other than those listed) rather than eating wheat based foods like pasta, pizza, sandwiches etc… I make a fruit smoothie every morning and juice fruits and veggies.
Vitamin C helps the body to reduce its load of vanadium and this has been studied for its possible role in treatment of bipolar disorder.35 A double-blind trial found that both manic and depressed bipolar patients were significantly improved after one-time administration of 3 grams of vitamin C, compared with a placebo.36 The same study found that both manic and depressed patients did better on a reduced-vanadium diet compared to a normal diet. Another double-blind study reported that 4 grams per day of vitamin C in combination with a drug known as EDTA (which also helps remove elements such as vanadium from the body) was helpful to depressed bipolar patients but not to those experiencing mania.37 Until more is known, people with bipolar illness should avoid supplements containing vanadium and consider supplementing with vitamin C.
http://www.vitacost.com/science/hn/Concern/Bipolar_Disorder.htm
Lee Thompson Young suffered from bipolar disorder before suicide: coroner’s report
 The ‘Rizzoli & Isles’ star, 29, was taking medication for bipolar disorder and was also suffering from depression when he shot himself in the head in August, a report from the Los Angeles County Coroner said. Lithium and Quetiapine Fumarate were detected in his blood, but no traces of opiates, alcohol, cocaine or other drugs were found in his system.
The ‘Rizzoli & Isles’ star, 29, was taking medication for bipolar disorder and was also suffering from depression when he shot himself in the head in August, a report from the Los Angeles County Coroner said. Lithium and Quetiapine Fumarate were detected in his blood, but no traces of opiates, alcohol, cocaine or other drugs were found in his system.
Lee Thompson Young, 29, was taking medication for bipolar disorder and was also suffering from depression when he killed himself in August, a report from the Los Angeles County Coroner said.
LOS ANGELES — The star of TNT’s “Rizzoli & Isles” who committed suicide in August had a history of bipolar disorder, authorities revealed Tuesday.
Lee Thompson Young, 29, was taking medication for the condition and also suffered from depression when he shot himself in his right temple while sitting on the couch of his North Hollywood bachelor apartment, a report from the Los Angeles County Coroner said.
“He was known to take his medications” and “appeared okay” when he last spoke with his doctor on Aug. 14, the report said.
Lithium capsules and Quetiapine Fumarate tablets were found in his residence, and both drugs were detected in his blood.
No traces of opiates, alcohol, cocaine or other drugs were found in his system.
Young was found Aug. 19 after he missed a call time on a production set and his manager requested a welfare check. The last time anyone spoke to him was Aug. 17.
Coroner officials said Young’s doctor was not aware of any financial problems or suicidal threats or attempts.
The gun recovered from the scene was a 40 caliber Sig Sauer semi-automatic registered to Young, the coroner report said.
The actor didn’t leave a suicide note, and his specific motive remains a mystery, officials said.
“He was ill. You don’t just do this,” a close friend who’s known Young since he was a teenager previously told the Daily News.
RELATED: LEE THOMPSON YOUNG DID NOT LEAVE SUICIDE NOTE: SOURCE
The friend said Young was religious, following the faith practiced by the Yoruba tribe of Nigeria and southern Benin.
He took a trip to a Yoruba village with him mom several months before his death and attended a “beautiful ceremony,” the friend said.
“He was very close to his mother and sister,” the friend said. “He had a great support network. He had his local priest and lots of good friends who were like family, including the ‘Rizzoli’ cast.”
The coroner report released Tuesday said investigators found a “makeshift altar” in Young’s closet with “miscellaneous religious items displayed.”
The friend said a prior media report linking Young’s depression to his faith was “a gross mischaracterization.”
 RELATED: FORMER DISNEY STAR LEE THOMPSON YOUNG DEAD AT 29
RELATED: FORMER DISNEY STAR LEE THOMPSON YOUNG DEAD AT 29
A better explanation, the friend said, is that Young was drawn to his faith because he yearned for enlightenment and may have been “too sensitive” for this world.
“He wouldn’t even play characters that were bad. He was all about good,” the friend said.
Production of the hit Boston police drama “Rizzoli & Isles” was temporarily halted after Young’s death.
“Everyone at ‘Rizzoli & Isles’ is devastated by the news of the passing of Lee Thompson Young. We are beyond heartbroken at the loss of this sweet, gentle, good-hearted, intelligent man,” TNT, Warner Bros. and executive producer Janet Tamaro said in a joint statement.
“He was truly a member of our family. Lee will be cherished and remembered by all who knew and loved him, both on- and off-screen, for his positive energy, infectious smile and soulful grace. We send our deepest condolences and thoughts to his family, to his friends and, most especially, to his beloved mother,” the statement said.
Young, originally from South Carolina, rose to fame in the leading role of the Disney Channel series “The Famous Jett Jackson” and also portrayed running back Chris Comer in the 2004 movie “Friday Night Lights.”
Actor Jordan Bridges, who plays Frankie Rizzoli, the onscreen brother of series co-star Angie Harmon, posted a final farewell on Twitter.
“Goodbye @Lee_T_Young,” Bridges tweeted in August. “I am shattered at your startling departure. It was an honor to work with you. Love and Prayers to your family.”
The Bipolar Cook
Fighting Depression with Culinary Arts
 When I walked into my sister’s house for Christmas this cake was sitting in the middle of the kitchen table. It looked so good that I had to share with you. This cake was made by my niece and brother-in-law, and when I asked him for the recipe or what he used, he could not remember, lol, go figure. So I decided to break it down on my own so that I could share it with you. This cake tasted like a peppermint patty. It was very good indeed. I have never been a big fan of candy canes, but this cake just works. It makes a wonderful conversation piece during the Holiday season, and using a simple butter cream frosting recipe, it is quite easy to put together. Enjoy!
When I walked into my sister’s house for Christmas this cake was sitting in the middle of the kitchen table. It looked so good that I had to share with you. This cake was made by my niece and brother-in-law, and when I asked him for the recipe or what he used, he could not remember, lol, go figure. So I decided to break it down on my own so that I could share it with you. This cake tasted like a peppermint patty. It was very good indeed. I have never been a big fan of candy canes, but this cake just works. It makes a wonderful conversation piece during the Holiday season, and using a simple butter cream frosting recipe, it is quite easy to put together. Enjoy!
1. You will need a big oven and 4 , 9″ rounds otherwise bake the cakes according to the box directions. Bake layers 2 at a time. Let cool on wire racks.
2. While cakes are cooling make the frosting. To make:
3. Beat butter for a few minutes with a mixer with the paddle attachment on medium speed.
4. Add 7 cups of powdered sugar and turn your mixer on the lowest speed (so the sugar does not blow everywhere) until the sugar has been incorporated with the butter.
5. Increase mixer speed to medium and add vanilla extract, salt, and 5 tablespoons of milk/cream and beat for 3 minutes.
6. If your frosting needs a more stiff consistency, add remaining sugar. If your frosting needs to be thinned out, add remaining milk or cream 1 tablespoons at a time.
7. Once your frosting is the consistency your looking for:
8. CONSTRUCT THE CAKE
9. Make sure the cake layers are trimmed and leveled. Set bottom layer onto a cake stand, frost top and sprinkle some crushed candy cane over the entire layer. Cover with second cake layer, frost top and begin to frost the sides of layers 1 and 2. Add candy cane pieces to top of layer two, then top with layer 3. Repeat process, once top cake layer is in place, frost the entire cake, and then press the candy cane pieces into the sides and top of cake.
10. And there ya have it. A super sized peppermint patty, that can feed and army!
 What Are Mixed Episodes in Bipolar Disorder?
What Are Mixed Episodes in Bipolar Disorder?Mixed episodes in bipolar disorder are a form of mental illness. In most forms of bipolar disorder, moods alternate between elevated and depressed over time. A person with mixed episodes experiences both mood “poles” — mania anddepression — simultaneously or in rapid sequence. Technically, mixed episodes are described only in people with bipolar I disorder (not bipolar II disorder), although this distinction is expected to change as the psychiatric diagnostic classification system is currently being revised.
Virtually anyone can develop bipolar disorder. About 2.5% of the U.S. population suffers from some form of bipolar disorder – nearly 6 million people.
Mixed episodes are common in people with bipolar I disorder. Estimates vary widely, but between 20% and 70% of people with bipolar disorder experience mixed episodes.
Those who develop bipolar disorder at a younger age, particularly in adolescence, may be more likely to have mixed episodes. People who develop mixed episodes may also develop “pure” depressed or “pure” manic or hypomanic phases of bipolar illness.
Most people are in their teens or early 20s when symptoms from bipolar disorder first start. Nearly everyone with mixed episodes develop bipolar disorder before age 50. People who have an immediate family member with bipolar are at higher risk.
Mixed episodes of bipolar disorder are defined by symptoms of mania and depression that occur at the same time, or in rapid sequence.
This may seem impossible — how can someone be manic and depressed at the same time? Because mixed manic episodes are a form of mental illness, they defy any predictable pattern of feelings or behavior.
For example, a person in a mixed manic episode could be crying uncontrollably while announcing they have never felt better in their life. Or they could be exuberantly happy, only to suddenly collapse in misery. A short while later they might suddenly return to an ecstatic state.
Mixed manic episodes can last from days to weeks or sometimes months, if untreated. Mixed episodes may recur and recovery can be slower than during episodes of “pure” bipolar depression or “pure” mania or hypomania.
The most serious risk of mixed bipolar disorder is suicide. People with bipolar disorder are 10 to 20 times more likely to commit suicide than people without bipolar disorder. Tragically, 8% to 20% of people with bipolar disorder eventually lose their lives to suicide.
Evidence shows that during mixed episodes, people may be at even higher risk for suicide than people in episodes of bipolar depression.
Treatment reduces the likelihood of serious depression and suicide. Lithium in particular, taken long term, reduces the risk.
People with bipolar disorder are also at higher risk for substance abuse. Nearly 60% of people with bipolar disorder abuse drugs or alcohol. Substance abuse is associated with more severe or poorly controlled bipolar disorder.
Mixed manic episodes generally require treatment with medication. Unfortunately, mixed episodes are more difficult to control than other episode types of bipolar disorder. The main drugs used to treat mixed manic episodes are mood stabilizers and antipsychotics.
Mood Stabilizers
Depakote is an antiseizure medication that also levels out moods. It has a more rapid onset of action, and in some studies has been shown to be more effective than lithium for the treatment of mixed episodes. Depakote is also sometimes used “off-label” for prevention of mixed manic episodes.
Some other antiseizure drugs, such as Tegretol, are also effective mood stabilizers.
Antipsychotics
Many atypical antipsychotic drugs are effective, FDA-approved treatments for mixed episodes. These include Zyprexa, Abilify, risperidone, Seroquel, Geodon, and Saphris. Antipsychotic drugs are also sometimes used alone or in combination with mood stabilizers for preventive treatment.
Electroconvulsive Therapy (ECT)
Despite its frightening reputation, electroconvulsive therapy (ECT) is an effective treatment for mixed manic episodes. ECT can be helpful if medication fails or can’t be used.
Treatment for Depression in Mixed Bipolar Disorder
Common antidepressants such as Prozac, Zoloft, and Paxil have been shown to worsen mania symptoms during mixed episodes without necessarily improving depressive symptoms. Most experts therefore advise against using antidepressants during mixed episodes. Mood stabilizers (particularly Depakote), as well as atypical antipsychotic drugs, are considered the first-line treatments for mixed episodes.
Mixed episodes of bipolar disorder often involve recurrences of mixed, manic, or depressed phases of illness. Therefore, it is usually recommended that medications be continued in an ongoing fashion to prevent relapses.
Reference: http://www.webmd.com
 Desiderata is latin for “desired things”
Desiderata is latin for “desired things”
Amazing and uplifting poem and there is even a spoken version by LazyBoy that is relaxing. I love it, hope you do to. For all those finding it hard to maintain peace in there lives as i know myself thats hard to do. Something positive to lift your spirit and your mind.
Poem:
Go placidly amidst the noise and haste, and remember what peace there may be in silence. As far as possible without surrender be on good terms with all persons. Speak your truth quietly and clearly; and listen to others, even the dull and the ignorant; they too have their story.
Avoid loud and aggressive persons, they are vexatious to the spirit. If you compare yourself with others, you may become vain or bitter; for always there will be greater and lesser persons than yourself.
Enjoy your achievements as well as your plans. Keep interested in your own career, however humble; it is a real possession in the changing fortunes of time.
Exercise caution in your business affairs; for the world is full of trickery. But let this not blind you to what virtue there is; many persons strive for high ideals; and everywhere life is full of heroism.
Be yourself. Especially, do not feign affection. Neither be cynical about love; for in the face of all aridity and disenchantment it is as perennial as the grass.
Take kindly the counsel of the years, gracefully surrendering the things of youth. Nurture strength of spirit to shield you in sudden misfortune. But do not distress yourself with dark imaginings. Many fears are born of fatigue and loneliness.
Beyond a wholesome discipline, be gentle with yourself. You are a child of the universe, no less than the trees and the stars; you have a right to be here.
And whether or not it is clear to you, no doubt the universe is unfolding as it should. Therefore be at peace with God, whatever you conceive Him to be, and whatever your labours and aspirations, in the noisy confusion of life keep peace with your soul. With all its shams, drudgery, and broken dreams, it is still a beautiful world. Be cheerful.
Strive to be happy.
Written
on June 10, 2014